With Halloween around the corner, friends and neighbors will do their best to send a shiver down your spine. But have you ever wondered what frightens dogs and cats?
Pets can develop fears and the exaggerated fears known as phobias. But unlike the make-believe ghosts and goblins of Halloween, some pets’ fears are so real that they can cause anxiety and lead to behavior problems, aggression or even property destruction and self-injury.
Fears can develop in an animal for many, many reasons, from traumatic experiences to genetics. But in pets, many common fears can be traced back to the ever-important socialization period of a pet’s early life. Fears may develop because of lack of exposure to people, places and situations during that socialization period, which is the first 12 weeks of life for dogs and the first 9 weeks for cats.
Common dog and cat fears
Both dogs and cats can develop a fear of just about anything. It may be rational, such as a pet that howls in fear during car rides after previous episodes of motion sickness. Or it can be apparently irrational, like the dog who shrieks every time the silverware drawer is opened.
Some pets are afraid of strangers and may bolt out of the room when the doorbell rings. Or they may come unglued when they meet a baby, a child, or a man in a uniform. Other pets may be frightened of other animals or of a specific breed of dog.
Certain situations, like a trip to the veterinary clinic or groomer, or a walk on slippery hardwood floors, can make pets shake in their paws. Pets can even be frightened by an unfamiliar object in the house, such as a new fan.
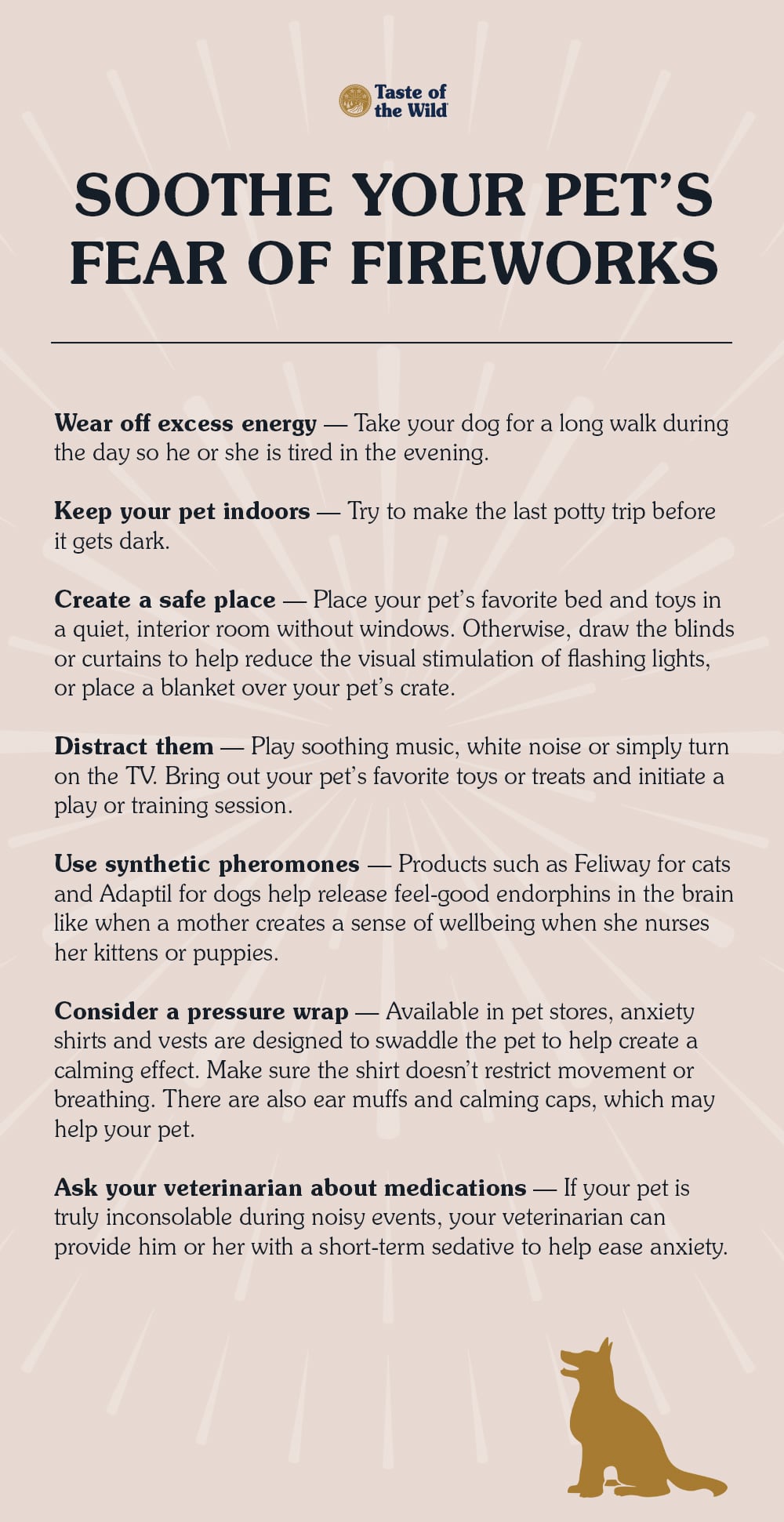
Common phobias in dogs include noise phobia, thunderstorm phobia and separation anxiety. Pets can also suffer from more than one phobia. In fact, many pets with thunderstorm phobia also have separation anxiety.
Signs of fear and anxiety
Fearful pets often feel anxiety, or a sense of unease in anticipation of a threat, that may be mild or severe.
Anxious dogs may pace, pant, drool and tremble. They often lick their lips and yawn. Cats can hiss and arch their backs, or they may nervously overgroom, resulting in hairless patches.
Both dogs and cats may freeze in place, hide, cower or try to make themselves appear small by curling into a ball, tucking their tails close and pinning their ears against their heads. Pupils are often dilated (enlarged), the hair on their spine may stand up and they may whimper or yowl. They may lose their appetites or become aggressive. Some may empty their anal glands or eliminate inappropriately.
These are all signs of a distressed pet, and under no circumstances should the pet be punished, which usually only exacerbates the pet’s fear and anxiety.
Overcoming Fears
The best way to help a fearful pet is to make an appointment with your veterinarian or a veterinary behavior specialist as soon as possible. They can work with you to help identify what’s causing your pet’s fear. They’ll also give your pet a thorough physical to make sure there aren’t any underlying medical problems that might contribute to the behavior. Typically, your veterinarian will recommend a combination of treatments, which may include behavior modification, environmental changes or, if needed, medications.
For the pet that runs when the doorbell rings, for example, you might start by changing the doorbell chime so it’s less likely to cause anxiety in your pet. Then, gradually desensitize the pet to the doorbell cue by asking family members to ring the bell and enter, so the pet recognizes that the sound results in a positive event. As your pet becomes more comfortable, provide a treat or toy each time they remain calm after the doorbell.
Then you can place your pet on a leash and gradually have other people your pet may be familiar with enter the door. Ask these people to ignore your pet and avoid eye contact. Treats may be tossed toward the pet to invite them to approach the person. In this way, work to gradually reduce the space between the person and the pet. Once your pet is comfortable with this, try having strangers come to the door, all the while rewarding your pet for non-fearful behavior.
Helping your pet overcome fears requires time, patience and positive reinforcement for every advancement he or she makes. But helping relieve anxieties can improve their quality of life, which makes it all worth it.